Pneumatic compression therapy, also known as intermittent pneumatic compression (IPC) can help prevent the formation of blood clots or DVTs (Deep vein thrombosis) in the deep veins of the legs.
Pneumatic compression devices consist of one or more compression sleeves attached to an air pump. The compression sleeves have a sequence of air pockets in them that can be set to inflate and deflate with varying pressures and different times. This way, the gentle pressure on the leg or arm helps improve blood flow in people who may be recovering from surgery or injury.
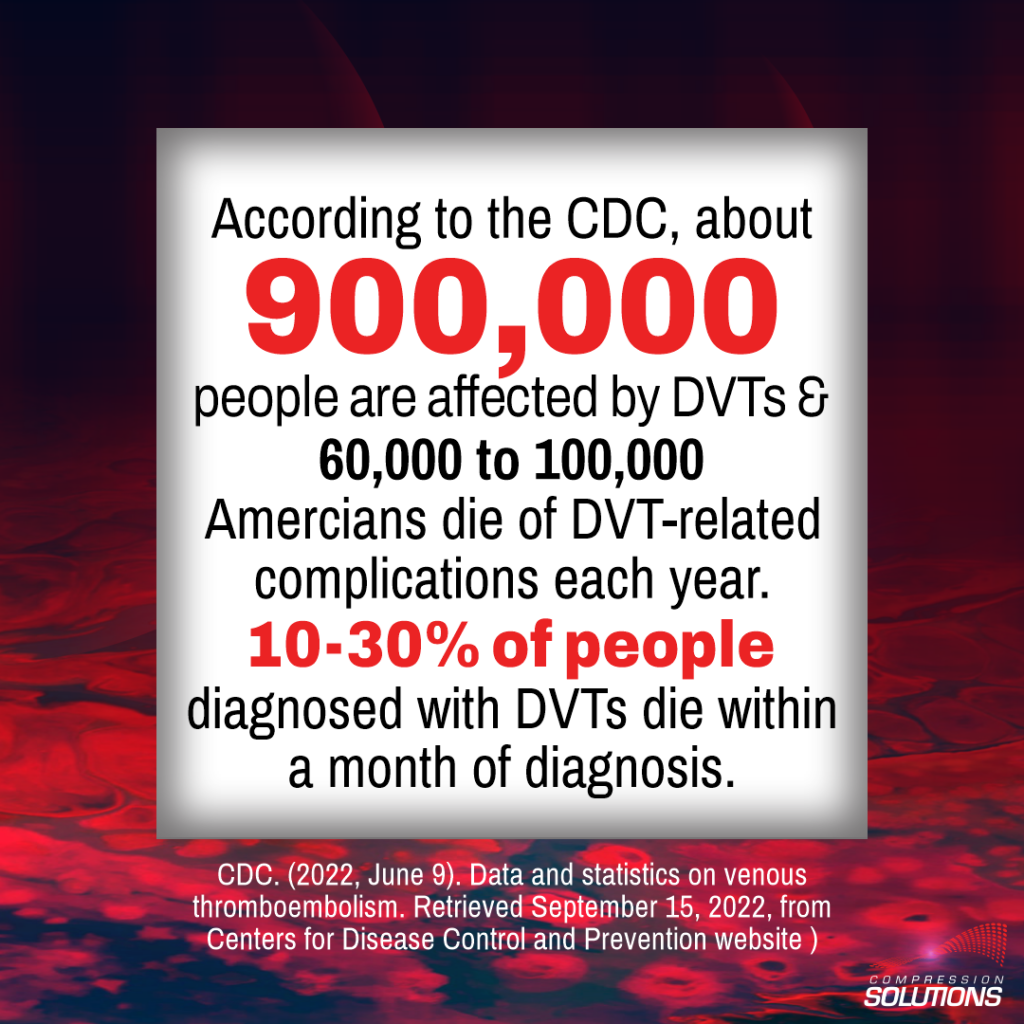
A DVT is a serious medical condition. According to the CDC, about 900,000 people are affected by DVTs and 60,000 to 100,000 Americans die of DVT-related complications each year. 10-30% of people diagnosed with DVTs die within a month of diagnosis1.
If you are at a high risk of developing DVTs, your provider may recommend pneumatic compression therapy during recovery after surgery or injury.
Why is there a risk of DVTs after surgery?
Our veins play an important role — they carry blood without oxygen back to the heart. Deep veins in our legs hold and transport 90-95% of the blood from the legs back to our heart. When the heart receives this blood, it adds oxygen to it, and our arteries pump oxygen-rich blood to our bodies. While blood flow in the arteries is pushed forward by the pumping action of the heart, veins do not have this luxury. Instead, veins need the muscles in our legs to squeeze blood through our veins.
Normally, this leg muscle compression happens when we walk, exercise, and move around. However, after surgery or injury, many people are forced to be inactive as they recover. This situation may cause blood circulation to slow down. For people with a high risk of developing DVTs, blood clots may form and cause a slew of health issues. A blood clot can break away and travel to the lungs and block blood flow, causing a pulmonary embolism (PE). PEs are dangerous and can be fatal.
Who is at risk of developing DVTs?
Your doctor will evaluate your medical history to determine your risk of developing DVTs (also known as VTEs or thromboembolism). In general, DVTs can be common in both men and women over 65 years of age. The risk of a DVT can be higher right after surgery when mobility gets affected and inflammation is high, or if a deep vein is injured. Some cancer therapy can also affect DVTs. Obesity and certain inherited blood disorders can also increase the risk of blood clots2.
Patients undergoing hip or knee surgery are at the highest risk of developing DVTs 2-10 days after surgery and the DVT risk remains for about three months.
In fact, without preventive treatment, up to 80% of orthopedic surgery patients will develop DVT and 10% will develop a PE3. This is why the American Academy of Orthopedic Surgeons (AAOS) recommends that surgeons use multiple ways to minimize the risk of DVTs4.
Based on your needs, these DVT prevention strategies may include blood thinners, anti-clotting medication, and pneumatic compression devices.
Do you need a pneumatic compression device after surgery?
Traditionally, most pneumatic compression devices were used in hospitals. Now that many surgeries are now outpatient procedures and devices are less expensive, they may also be used at home. Your healthcare provider will recommend the right type of pneumatic compression device for you, based on your needs.
There are different types of pneumatic compression devices. The sleeve may cover the entire leg or a part of it. The pneumatic (air) pockets can be programmed in different ways to inflate and deflate based on the device. Some devices allow a sequential compression, while others have cuffs that allow select air pockets to be inflated around the leg. Advanced solutions even offer the benefits of cold compression along with physical compression (mechanical prophylaxis).
Cold compression can help reduce pain and swelling after surgery, and accelerate recovery after surgery. For example, Triple Play VT offers cold compression and helps reduce the risk of DVTs/VTEs5-8.
